Or, “What are they saying?“
When we mention the word Serotonin (5-hydroxytryptamine, 5-HT), we immediately think of the brain and the Central Nervous System (CNS). People tend to associate serotonin to depression, or mood, or feelings of well-being1.
Although that is correct, truth be told, the majority of the serotonin in the human body is actually produced in the gut. In fact, 95% of total serotonin is manufactured by the Enterochromaffin cells (or, Kulchitsky cells) in the gastro-intestinal tract (GI)2,3. These cells live next to the gut epithelium, that covers the cavity of the GI tract, playing a crucial role in the regulation of bowel movements and secretions. If you think that the gut is almost 9 meters (or 30 feet) long, then that’s a lot of cells producing serotonin.
When in the 50’s, Betty M. Twarog and Irvine H. Page discovered that the brain produced its own serotonin4; then, the gut-made serotonin got reduced to its “Aschenputtel” origins, and relinquished to the favela quarters of the body. As such, brain-derived serotonin always got more attention than its gut-derived counterpart – like a rich vs. poor-cousin type of reputation.
Moving-on…
Platelets, also called thrombocytes, are small un-nucleated fragment of cells that, when activated, form blood clots (thrombus) and prevent bleeding.
Platelets do not make serotonin, butcan take it up as they circulate through the gut, and carry it along the blood stream6,7. As such, the serotonin produced in the intestine can be carried all over the body. As the chemical messenger serotonin is, it can influence any other cell, in whatever other location, as long as it has a serotonin receptor on it. As such, peripheral serotonin has now discovered its path back into the limelight, and recent research has strengthened the influence that gut-made serotonin has in other parts of the body, functioning as an intestinal-derived hormone.
Once again, the “Aschenputtel” story comes into mind, but this time through its “Cinderella” version. Let’s take a look…
For example, gut-derived serotonin can directly regulate the liver and mediate liver regeneration8. In Non-Alcoholic Fatty Liver Disease (NAFLD), a group of conditions that are characterized by excessive fat accumulation in the liver and closely track the global public health problem of obesity, researchers showed that inhibiting gut-derived serotonin synthesis could resolve hepatic fat accumulation8,9.
Peripheral serotonin can also be a negative regulator of bone density, by specifically inhibiting osteoblast formation and leading to osteoporosis10 – a common feature in patients with inflammatory bowel disease (IBD). This happens through the action of a common receptor: the low-density Lipoprotein Receptor-related Protein 5(LRP5), which is expressed in both osteoblasts and enterochromaffin cells11. LRP5 inhibits the expression of an important ingredient for serotonin production (Tryptophan hydroxylase-1, Tph1); as such, when LRP5 is deficient or inactivated due to inflammation or disease, blood levels of serotonin are elevated decreasing osteoblast formation; and, consequently, reducing bone mass1,11.
Epidemiologic data suggests a role of serotonin, or Selective Serotonin-Reuptake Inhibitors (typically used as antidepressants, SSRIs) in the development of venous thrombosis12. In fact, patients with depression were reported to have higher incidences of venous thromboembolism in general13; and, the use of SSRIs is associated with an increased venous thromboembolism risk14. No wonder, serotonin and platelets are “brothers in arms”, ready to block any blood vessel along their way….
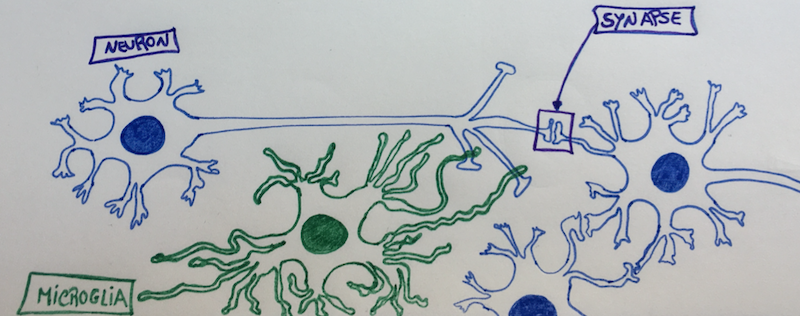
Serotonin and its receptors are also present in the immune system, where evidence suggests it contributes to both innate and adaptive responses. There is now clear evidence of a straight communication between the immune system, the gut and the brain via serotonin15,16.
On top of all and because we are not alone, our gut microbiota plays a critical role in regulating our colonic serotonin. Indigenous spore-forming bacteria (Sp) promote serotonin biosynthesis in our enterochromaffin cells, and with that they can significantly modulate GI movements and platelet function – together with many aspects of our physiology17,18. We now know that the microbiota colonizes the GI tract after birth, with a continuous maturation during the first years of life19. Researchers have now showed in animal models that this developing gut microbiota regulates the development of the adult enteric nervous system via intestinal serotonin networks20. What this actually means, is that the actions of our intestinal bugs during the beginning of our life are determinant for the development of our “gut brain”, our second brain. How about that?…
If we ruminate about it, when we “think” with our gut, we are actually listening to our bugs. By directly signalling our cells to produce serotonin and develop a network of neurons as soon as we are born, our gut-bugs are actually finding a way to communicate with us – the host – in the serotonin language.
Now, we just need to understand what are they telling us…
References:
1 Gershon, M. D. 5-Hydroxytryptamine (serotonin) in the gastrointestinal tract. Curr Opin Endocrinol Diabetes Obes 20, 14-21, doi:10.1097/MED.0b013e32835bc703 (2013).
2 Bellono, N. W. et al. Enterochromaffin Cells Are Gut Chemosensors that Couple to Sensory Neural Pathways. Cell 170, 185-198.e116, doi:10.1016/j.cell.2017.05.034 (2017).
3 Yaghoubfar, R. et al. Modulation of serotonin signaling/metabolism by Akkermansia muciniphila and its extracellular vesicles through the gut-brain axis in mice. Scientific Reports 10, 22119, doi:10.1038/s41598-020-79171-8 (2020).
4 Twarog, B. M. & Page, I. H. Serotonin Content of Some Mammalian Tissues and Urine and a Method for Its Determination. American Journal of Physiology-Legacy Content 175, 157-161, doi:10.1152/ajplegacy.1953.175.1.157 (1953).
5 Zilla, P. et al. Scanning electron microscopy of circulating platelets reveals new aspects of platelet alteration during cardiopulmonary bypass operations. Tex Heart Inst J 14, 13-21 (1987).
6 Morrissey, J. J., Walker, M. N. & Lovenberg, W. The absence of tryptophan hydroxylase activity in blood platelets. Proc Soc Exp Biol Med 154, 496-499, doi:10.3181/00379727-154-39702 (1977).
7 Hughes, F. B. & Brodie, B. B. The mechanism of serotonin and catecholamine uptake by platelets. J Pharmacol Exp Ther 127, 96-102 (1959).
8 Wang, L. et al. Gut-Derived Serotonin Contributes to the Progression of Non-Alcoholic Steatohepatitis via the Liver HTR2A/PPARγ2 Pathway. Frontiers in Pharmacology 11, doi:10.3389/fphar.2020.00553 (2020).
9 Choi, W. et al. Serotonin signals through a gut-liver axis to regulate hepatic steatosis. Nature Communications 9, 4824, doi:10.1038/s41467-018-07287-7 (2018).
10 Lavoie, B. et al. Gut-derived serotonin contributes to bone deficits in colitis. Pharmacol Res 140, 75-84, doi:10.1016/j.phrs.2018.07.018 (2019).
11 Yadav, V. K. et al. Lrp5 controls bone formation by inhibiting serotonin synthesis in the duodenum. Cell 135, 825-837, doi:10.1016/j.cell.2008.09.059 (2008).
12 Rieder, M., Gauchel, N., Bode, C. & Duerschmied, D. Serotonin: a platelet hormone modulating cardiovascular disease. J Thromb Thrombolysis 52, 42-47, doi:10.1007/s11239-020-02331-0 (2021).
13 Takeshima, M. et al. Prevalence of Asymptomatic Venous Thromboembolism in Depressive Inpatients. Neuropsychiatr Dis Treat16, 579-587, doi:10.2147/NDT.S243308 (2020).
14 Parkin, L. et al. Antidepressants, Depression, and Venous Thromboembolism Risk: Large Prospective Study of UK Women. J Am Heart Assoc 6, doi:10.1161/jaha.116.005316 (2017).
15 Baganz, N. L. & Blakely, R. D. A dialogue between the immune system and brain, spoken in the language of serotonin. ACS Chem Neurosci 4, 48-63, doi:10.1021/cn300186b (2013).
16 Jacobson, A., Yang, D., Vella, M. & Chiu, I. M. The intestinal neuro-immune axis: crosstalk between neurons, immune cells, and microbes. Mucosal Immunology 14, 555-565, doi:10.1038/s41385-020-00368-1 (2021).
17 Yano, J. M. et al. Indigenous bacteria from the gut microbiota regulate host serotonin biosynthesis. Cell 161, 264-276, doi:10.1016/j.cell.2015.02.047 (2015).
18 Reigstad, C. S. et al. Gut microbes promote colonic serotonin production through an effect of short-chain fatty acids on enterochromaffin cells. Faseb j 29, 1395-1403, doi:10.1096/fj.14-259598 (2015).
19 Bäckhed, F. et al. Dynamics and Stabilization of the Human Gut Microbiome during the First Year of Life. Cell Host Microbe 17, 690-703, doi:10.1016/j.chom.2015.04.004 (2015).
20 De Vadder, F. et al. Gut microbiota regulates maturation of the adult enteric nervous system via enteric serotonin networks. Proc Natl Acad Sci U S A 115, 6458-6463, doi:10.1073/pnas.1720017115 (2018).